According to the Code of Professional Conduct for Case Managers, a board-certified case manager’s (CCM’s) primary ethical responsibility is to advocate for his/her clients, which at least entails advocating for the benefits that clients are reasonably owed.
Unfortunately, your obligation to advocate for goods or services not enumerated in the client’s health insurance policy can be problematic. In such instances, the case manager ought simply to exercise his or her best judgment.
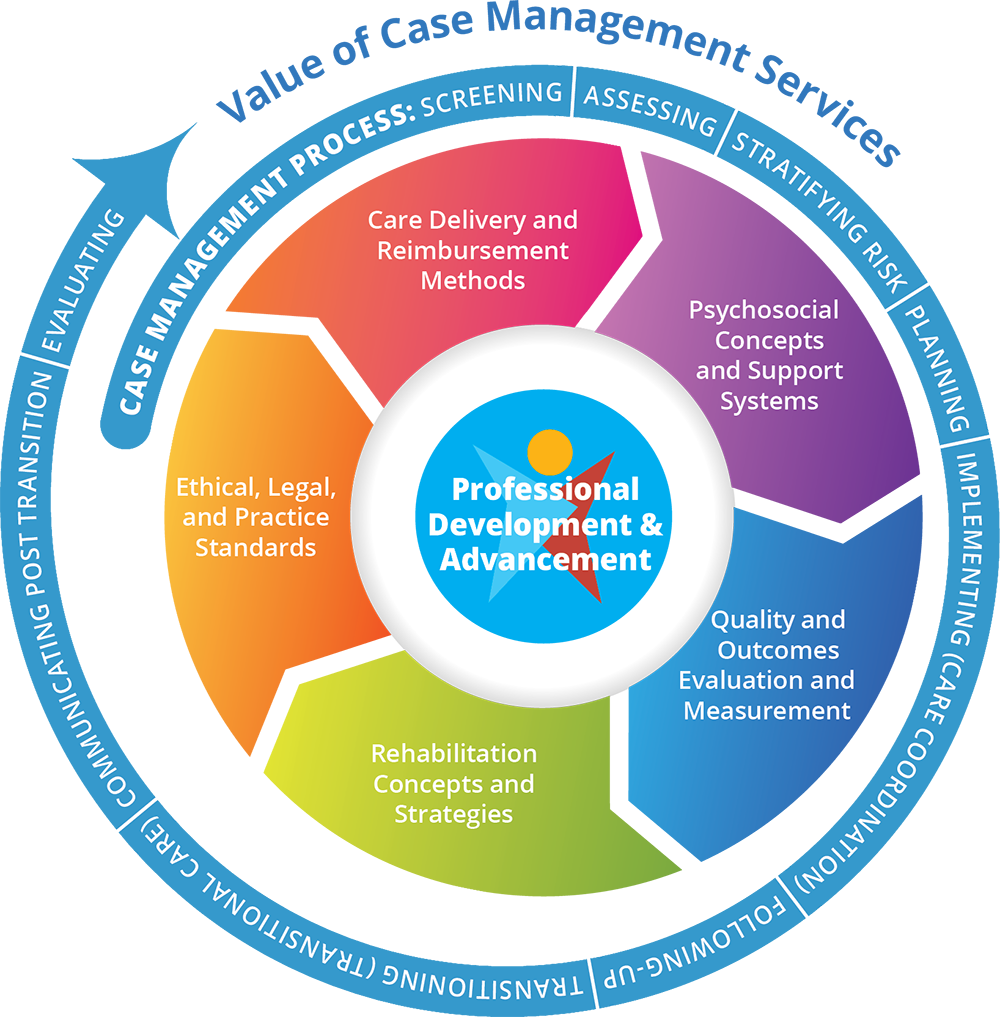
You may use the “Quadrant Model” (Jonsen, Siegler, & Winslade, 2006) for guidance on how to navigate moral judgment. Jonsen, Seigler, and Winslade divide moral reflection into four categories or quadrants.
The Quadrant Model of Moral Judgment
In this quadrant model, you as the moral decision maker analyze ethical dilemmas according to four main aspects of the situation your client/support system is facing. You use the various quadrants’ guidelines to inform your ethical reasoning and resolutions.
Focus Areas of the Quadrant Model of Moral Judgment
| Quadrant | Area of Special Focus |
|---|---|
| Medical and clinical information | The client’s clinical and medical condition and circumstance in general. |
| Client’s preferences | What the client/support system desires in terms of options for healthcare services. This also considers the client’s ability to make decisions that are consistent with his/her own authentic desires and wishes. |
| Contextual features | The ways the client’s familial circumstances, spiritual orientation, religious beliefs, or economic resources may be important considerations in resolving ethical disputes. |
| Quality of life | The way health insurance benefits affect the options for healthcare services which ultimately influence the client’s quality of life. This also refers to the healthcare professional’s (i.e., case manager’s) primary responsibility to foster the client’s quality of life. |
First Quadrant: Client’s Information Based on Medical and Clinical Condition
This quadrant of moral judgment simply emphasizes the client’s clinical, medical, and general circumstances. In this regard, you seek to answer the following questions:
- What is the nature of the client’s disease, its history, its associated diagnosis and prognosis?
- What treatments, intervention, services, and resources are available?
- What are the success probabilities of the various available treatments, interventions, and resources?
- What are the various ways “success” might be understood?
All of these are “what”-type questions – they seek to factually comprehend all the clinically relevant details of the client/support system’s situation. But despite being facts rather than ethical “shoulds” or “oughts,” they can nevertheless have a huge impact on ethical reasoning. Consider the following examples:
- Data shows that a standard generic drug would appear to work every bit as well as a new but very expensive version of the drug. This should incline you to recommend using the former rather than the latter version.
- A client who needs an organ transplant but has no support network – which would be needed for post transplant care – may influence whether you pursue the transplant, despite the client’s level of need.
Knowing the facts affecting a client’s care can have an enormous bearing on the ultimate decision as to whether or not to allocate a benefit and whether or not that allocation is “just.”
Second Quadrant: Client’s Preferences
This returns us to the earlier considerations on autonomy and the client’s ability to make decisions that are consistent with his/her authentic desires, preferences, and wishes. In your role as case manager, recall that:
- Clients who are judgmentally and cognitively able have the autonomous right to make medically unwise decisions (e.g., refuse a treatment or service).
- As a healthcare professional you are obligated to accommodate the client’s preferences to which he/she is reasonably entitled.
- In instances in which someone else is making decisions for the client (e.g., a member of the client’s support system or a designated healthcare proxy), you must be careful that the decision maker is legally authorized to do so. Many states have laws as to who can consent for individuals who are cognitively impaired, and you should be thoroughly informed about them.
As case manager you incorporate clients’ preferences into your case management plans of care. You also exercise shared decision making to ensure that these plans meet your clients’ needs.
For example, when designing the plan of care, case managers consider the following client characteristics that influence the case management and care approach:
Client Characteristics
| Examples of Client Characteristics that Influence Preferences |
|---|
|
|
|
|
|
|
|
|
|
Third Quadrant: Client’s Quality of Life
This quadrant revisits the quandaries surrounding how the benefits of the care provided to clients might be evaluated when there are disputes about whether X is a health insurance benefit included in a client’s health plan or not. Some questions you may consider are:
- When is a health insurance benefit no longer a “benefit” (e.g., there is confusion whether the client has exhausted a particular benefit)?
- How do you choose among competing benefits when not all are available (e.g., the client has a primary and a secondary insurance policy and it is unclear which of the policies is best to use for coverage)?
- How much benefit is a client/support system owed?
- Are there any disputes about the benefits with the client’s health insurance agency (i.e., payor)?
Scholars and health economists have devised various metrics for addressing these questions such as cost-effectiveness analysis, cost-benefit analysis, and quality of adjusted life-years.
A primary responsibility of yours – as with other healthcare professionals – is fostering the client’s quality of life. However, a central problem is that ethical issues associated with quality of life recognize that people can markedly disagree on what constitutes an acceptable quality of life.
A common problem – if not the most common – confronting ethics committees in healthcare organizations is an exasperated healthcare team that pleads to withhold, withdraw, or de-escalate life-prolonging treatment for a particular client when the client’s support system wishes the opposite.
End-of-Life and Quality-of-Life Care: An Ethical Conflict
| Case Scenario | Commentary |
|---|---|
|
You are a case manager on a healthcare team caring for Mr. Jensen, who has a terminal illness. Mr. Jensen is on life support, unconscious, and unresponsive to the treatment. In the team’s opinion, Mr. Jensen’s treatment is no longer serving any real benefit but only prolonging his suffering. Mr. Jensen’s immediate family members including his healthcare proxy, on the other hand, are adamant that aggressive, life-prolonging treatment be continued. They argue that their religious faith inclines them to believe that a miracle will occur, and any additional life at all, regardless of its quality, is infinitely precious. Although Mr. Jensen had appointed a healthcare proxy prior to the current episode of illness, documentation of the healthcare proxy lacks important details, especially those that speak to the conditions of when to terminate life support or aggressive treatment. |
In the midst of such end-of-life care scenarios you may feel immense frustration – and for good reason. You can certainly sympathize with a healthcare team that wants to de-escalate treatment because they feel they are only harming Mr. Jensen by prolonging his suffering. However, Mr. Jensen’s family members and proxy can, nevertheless, exert enormous authority over the nature and scope of end-of-life care their loved one receives.
Both ethical and legal reasoning allow Mr. Jensen’s family members and proxy acting in good faith to best represent how Mr. Jensen would understand his quality of life, and therefore to best represent what he would have wanted. Because respect for client autonomy is prominent in our ethical reasoning, healthcare professionals who differ from family members on the client’s quality of life usually have their opinions trumped by the client’s representatives – in this case Mr. Jensen’s family and healthcare proxy. Unless you can show that the treatments in question are physiologically futile (i.e., the treatments are known to be unable to secure the hoped-for outcome and therefore are simply wasted on the client), courts will usually side with the family’s, surrogate’s, or proxy’s wishes (Texas courts being a notable exception). |
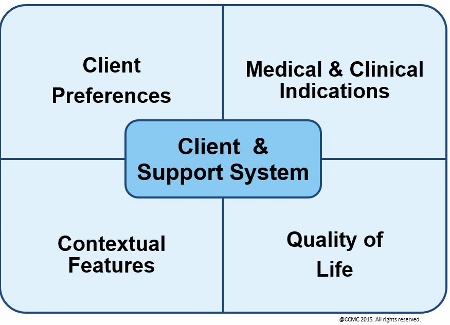
Fourth Quadrant: Contextual Features
This quadrant refers to the ways the client’s support system circumstances, psychosocial network, spiritual orientation, religious beliefs, or economic resources function as important considerations in resolving ethical conflicts or disputes. It also refers to the characteristics of the external environment as well, such as laws, regulations, and access to healthcare resources and services.
Two Categories of Contextual Features
For example, knowing that a client is very religious might enable you to include sources of spiritual comfort and strength in the client’s case management plan of care. Including such contextual features in the client assessment contributes to the development of effective case management plans of care, which ultimately reduces potential for ethical conflict.
Knowledge of a client’s hobbies or intellectual pursuits may enable rapport and trust to develop between you and your client/support system. Especially important – as virtually every case manager appreciates – is knowing the degree of support that a client will likely receive from immediate members of the client’s support system, as this can be enormously important in planning and coordinating the client’s care program.
 One of the most significant contextual features in a client’s case management plan of care can be applicable federal, state, and local laws and regulations.
One of the most significant contextual features in a client’s case management plan of care can be applicable federal, state, and local laws and regulations.
The nature of relevant case law and regulations can affect the scope of an individual’s health insurance benefits, the content of his/her living will or durable power of healthcare, and the client’s confidentiality and privacy. In addition to your ethical insight, you should be reasonably familiar with the ways relevant laws and regulations pertain to your client’s care, as the failure to do so could result in any number of unpleasantries – both ethical and legal.
Because your primary role is to advocate for clients/support systems, you must be ultra-sensitive to the ethical dilemmas you might face, and you must know where to go for resources. Any or all of the following can be of enormous assistance to your case management duties:
- Trustworthy colleagues
- Legal resources and counsel
- Clinical experts
- Ethicists
- Supervisors
- Codes of ethics and professional conduct
In addition, as a board-certified case manager, you can contact the CCMC Committee on Ethics and Professional Conduct for an ethical opinion. You are not required to give the committee detailed descriptions of your real-life ethical dilemma, but you can put a question to the committee generally or hypothetically.
Consider the following example: “Suppose a case manager had a client who was in situation X, and the case manager also realized that Y was occurring. Are there certain ethical standards or principles that she should particularly keep in mind in going forward with caring for this client?”
That cases can be discussed as hypotheticals may relieve you of the fear that you would be breaching your client’s confidentiality and privacy – a fear that might otherwise lead you to believe you are barred from seeking external advice.
Whether you participate in continuing education programs voluntarily or to meet a requirement imposed upon you by your credentials (e.g., case management certification), these activities offer you the opportunity to keep current with ethical case management practice. As many case managers do, you may not only attend continuing education courses and programs, but also consider playing leadership roles in your local or regional professional case management associations.
The continuing education events and involvement in professional organizations are excellent opportunities for discussing ethical issues. Case study analyses, recent ethical and legal developments affecting case management, and the ethical challenges of new drugs, devices, and technologies can be discussed at such forums – perhaps by panels of experts.
You should be especially keen to understand how your informed or knowledgeable peers would manage ethically fraught situations, because the nature of an ethically “reasonable” solution to a problem is often represented by what a fair sampling of one’s colleagues or peers would do (the prudent and reasonable).
General Considerations for Effective Ethical Action
| Issue | Sample Questions that Assist Case Managers in Ensuring Effective Ethical Action |
|---|---|
| General |
|
| Autonomy |
|
| Nonmaleficience |
|
| Beneficence and justice |
|
| Veracity |
|
| Quadrant model |
|
Today’s case managers face an extraordinary array of ethically challenging situations. The following require you to be especially ethically thoughtful, competent, and well informed:
- New drugs
- New medical devices
- Experimental treatments and therapies
- New technologies
- New legislation on healthcare delivery and reimbursement
- Evolving demographics of healthcare consumers